


 |  |  |
| | ||
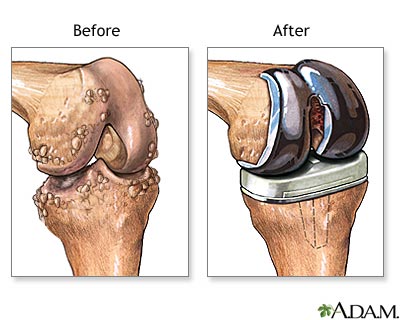
Knee joint replacement - series: Aftercare
 |
|
You will return from surgery with a large dressing to the knee area. A small drainage tube will be placed during surgery to help drain excess fluids from the joint area. Your leg will be placed in a continuous passive motion (CPM) device (a mechanical device that flexes (bends) and extends (straightens) the knee at a pre-set rate and amount of flexion).
Gradually, the rate and amount of flexion will be increased as tolerated. The leg should always be in this device when in bed. The CPM device helps speed recovery, decreases post-operative pain, bleeding and infection.
You will experience moderate pain after surgery. However, you may receive patient-controlled analgesia (PCA), or epidural analgesics to control your pain for the first 3 days after surgery. The pain should gradually decrease, and by the third day after surgery, oral analgesic medications may be sufficient to control your pain.
Try to schedule your pain medications about one half hour before walking or position changes. You will also return from surgery with several IV lines in place to provide hydration and nutrition. The IV will remain in place until you are taking adequate amounts of oral fluids.
Prophylactic (preventive) antibiotics may be given to reduce the risk of developing an infection, necessitating removal of the artificial joint.
You will also return from surgery wearing anti-embolism stockings or an inflatable pneumatic compression stockings. These devices are used to reduce your risk of developing blood clots, which are more common after lower extremity surgery.
Additionally, you will be encouraged to start moving and walking early after surgery. You will be assisted out of bed to a chair on the first day after surgery. When in bed, bend and straighten your ankles frequently to prevent development of blood clots.
Update Date: 7/23/2008 Updated by: Neil J. Gonter, MD, Assistant Professor of Medicine, Columbia University, New York, NY, and private practice specializing in Rheumatology at Rheumatology Associates of North Jersey, Teaneck, NJ. Review provided by Verimed Healthcare Network. Also reviewed by David Zieve, MD, MHA, Medical Director, A.D.A.M., Inc.
